PELVIC CONGESTION SYNDROME MELBOURNE
OVARIAN VEIN EMBOLISATION
Learn about Pelvic Congestion Syndrome and Ovarian Vein Embolisation treatment including the procedure, benefits, risks and more:
OVARIAN VEIN EMBOLISATION MELBOURNE
Source: Dr Philip Chan – MBBS, MMed (Radiology), FRANZCR, EBIR.
Interventional Radiologist.
WHAT IS PELVIC CONGESTION SYNDROME
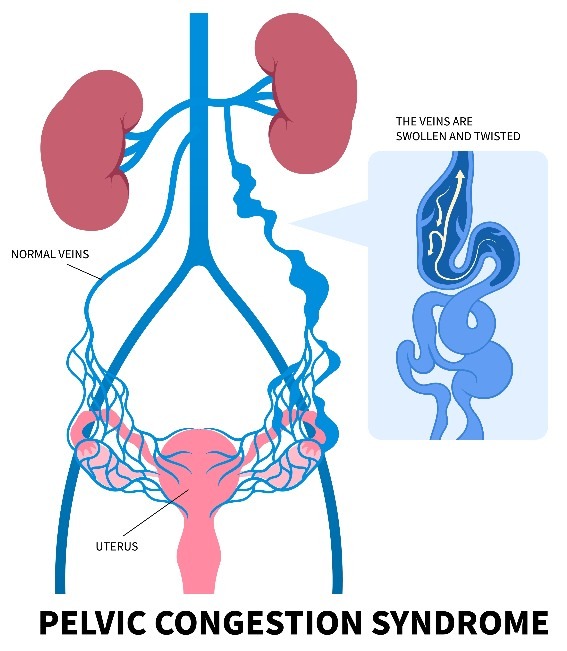
Pelvic Congestion Syndrome is a complex chronic condition. It is one of many potential causes of chronic pelvic pain.
Typical symptoms include dull, aching pelvic heaviness or dragging sensation (relieved by lying down) or pain during sexual intercourse.
Symptoms are non specific and can be caused by other problems such as fibroids, adenomyosis, endometriosis, urinary or bowel problems.
Diagnosis of Pelvic Congestion Syndrome is often made after careful specialist assessment, medical imaging and exclusion of other causes of these symptoms.
A common cause of Pelvic Congestion Syndrome is primary ovarian vein incompetence, characterised by abnormal blood flow of the ovarian and uterine veins without underlying causes such as blockage or narrowing of the veins.
Pelvic Congestion Syndrome typically affects women who have had multiple pregnancies, as hormonal changes and pressure on pelvic veins can contribute to the condition.
Source: IRSA – Ovarian Vein Embolisation
WHAT IS AN OVARIAN VEIN EMBOLISATION AND HOW IS IT PERFORMED
An Ovarian Vein Embolisation is a minimally invasive operation used to treat primary ovarian incompetence.
The procedure is performed through a 2-3 mm hole through a vein in the groin or neck. A catheter, a small hollow plastic tube, is placed into the ovarian and pelvic veins and the blood flow assessed.
If ovarian vein incompetence is confirmed, the vein is blocked with a combination of coils and a medical grade irritant which causes the vein to clot.
The operation typically takes 45 minutes to an hour, and can be safely performed under sedation and local anaesthesia.
All coils used in the embolisation are sterile, medical grade coils. Most coils are made with platinum or an alloy of platinum and tungsten. Once placed, they will remain in your body permanently.

Source: IRSA – Ovarian Vein Embolisation
ADVANTAGES OF AN OVARIAN VEIN EMBOLISATION
An Ovarian Vein Embolisation procedure has the following advantages:
Highly effective treatment for PCS, with an 83% success rate.
Minimally invasive procedure – Small incisions 1.5mm – 3mm
Faster recovery time compared to traditional open surgical approach.
Fewer risks compared to a traditional open surgery.
Shorter hospital stay than traditional surgery.
It’s important to consult a specialist to ensure that ovarian vein embolisation is the right treatment for your specific condition.
HOW TO PREPARE FOR AN OVARIAN VEIN EMBOLISATION
Preparing for a Ovarian Vein Embolisation – Your doctor and the WIRES Radiology team will discuss with you the procedure process and hospital administration needs.
Investigations and tests – You may require more relevant investigations such as blood tests, ultrasound, CT or MRI as part of your preparation for the procedure.
Fasting and overnight hospital stay – Generally, you are required to fast for 6 hours before the procedure. Please prepare for an overnight hospital stay (even if you are expecting to be discharged the same day).
Medications – Your doctor will review your list of medications and advise which medications you may need to stop before the procedure and when you may resume taking them again.
Going home – Remember to organise someone to drive you home after your operation.
RECOVERY – AFTER AN OVARIAN VEIN EMBOLISATION
Going home – Most patients can expect to go home the same day.
Pain & pain management – You will experience some abdominal and back pain. These side effects are expected to resolve in a few weeks and may be managed with over the counter pain killers such as paracetamol and ibuprofen.
Activity levels – You will be asked to refrain from exerting yourself, carrying heavy objects (up to 5 kg) or having sex for a week as they may cause the veins to “open up”.
Medications – Your doctor will discuss your medications with you and if/when to stop or start taking them after your prodcedure.
Post embolisation syndrome – Post embolisation syndrome is caused by the body’s reaction to the procedure. Patients often feel fatigued, have low grade fever, nausea, vomiting, low appetite, generalised muscle and joint aches – similar to having a cold without the head symptoms.
These are easily managed with paracetamol and ibuprofen, and should resolve after 7-14 days.
FREQUENTLY ASKED QUESTIONS
Immediately after the operation – You’ll be observed for a few hours post-procedure and most patients can usually go home the same day of their operation.
Pain management – Most patients may experience mild pelvic discomfort, which can be managed with over-the-counter medications.
Full recovery from ovarian vein embolisation side effects typically occurs within 7-14 days.
Improvement timeline – Improvement can begin within weeks, though the full benefits may take up to six months. Some patients may notice mild discomfort during their next menstrual cycle as the body adjusts.
Every patient is different, so your response to the treatment may vary. Your doctor will guide you through what to expect during recovery and provide follow-up care advice as necessary.
Risks – Like any medical procedure an Ovarian Vein Embolisation carries certain risks. Whilst the procedure is generally safe, potential risks may include:
- Bruising at the site of the catheter insertion
- Back and pelvic ache
- Rare complications like allergies or vascular injury
- In very rare cases, a coil used in the procedure may migrate to the lung, potentially causing a mild cough or chest discomfort.
These instances are uncommon, and the benefits of this minimally invasive treatment often outweigh the risks for those suffering from Pelvic Congestion Syndrome.
Your doctor will outline all the risks specific to your situation.
An Ovarian Vein Embolisation is generally well-tolerated as it is a minimally invasive procedure.
Patients receive a local anaesthetic at the insertion site, and many patients experience only mild discomfort afterward.
Most pain typically resolves within two weeks and can be managed by most patients with over the counter pain medication.
An Ovarian Vein Embolisation is a minimally invasive interventional radiology treatment and is considered safe. Most patients do not experience long-term side effects. Follow-up with your doctor or interventional radiologist is essential to ensure the best possible outcome.
Your doctor will fully explain the procedure and any potential side effects and mitigation strategies to make you as comfortable as possible during and after the procedure.


